Information & Common Questions
What Is Diabetes?
Humans normally control blood sugar (glucose) within a narrow range. After eating, the pancreas produces a hormone called insulin to help transport glucose from the blood stream to tissues in the body which require energy (e.g. muscle). Diabetes mellitus is a condition where the body is unable to control sugar levels, either because the pancreas does not produce insulin or cannot produce enough to keep glucose levels in check.
What is the difference between type 1 diabetes and type 2 diabetes?
Type 1 diabetes typically develops in children and young adults, although it can, less commonly, present in older adults. Type 1 diabetes is caused by the body's immune system destroying insulin producing cells in the pancreas (beta cells). All patients with type 1 diabetes require insulin injections to treat the condition effectively.
Type 2 diabetes typically develops in adults and is associated with obesity. However not all patients with type 2 diabetes are obese and, indeed, not all obese individuals develop type 2 diabetes. Patients susceptible to developing type 2 diabetes are often resistant to insulin, meaning they need to produce large quantities of insulin to maintain normal glucose levels. Over time, the pancreas is unable to maintain production of insulin and, at this stage, glucose levels rise and diabetes develops. Most patients with type 2 diabetes can initially be managed with lifestyle advice (diet and exercise to produce weight loss) and tablets. However patients with type 2 diabetes often require insulin therapy when their glucose levels are no longer controlled by lifestyle and tablets.
Why is diabetes important?
In the short term (days and weeks), uncontrolled diabetes (high blood glucose levels) can result in a range of symptoms including: extreme thirst, frequent urination (including waking through the night to use the toilet), tiredness and weight loss. Gaining control of blood glucose causes rapid resolution of these symptoms.
In the longer term (years), poorly controlled blood glucose levels can increase the chance of developing complications related to diabetes. Exposure to high blood glucose levels over a long period of time can result in damage to the eyes (retina), kidneys and nerves. Patients with diabetes are also at greater risk of cardiovascular disease. However, with appropriate diabetes care, the chances of developing complications can be dramatically reduced.
What is HbA1c?
HbA1c (Haemoglobin A1c, also known as glycated haemoglobin) is a blood test used in clinic to determine how well controlled blood glucose levels have been in patients with diabetes. Glucose sticks to red blood cells in the circulation and the higher the glucose level, the more glucose sticks to haemoglobin on the red blood cells. Because red blood cells have a lifespan of around 120 days, HbA1c provides useful information as to what a patient’s average blood glucose level has been over a 2 to 3 month period. This is different from a finger-prick glucose test which only provides information on the blood level at that particular moment.
The target HbA1c will differ depending on the individual and should be agreed between the patient and their diabetes team. Intensive (or tight) control of diabetes is often described as an HbA1c between 6.5 and 7.5% (48 – 58 mmol/mol) but this is not appropriate for all patients.
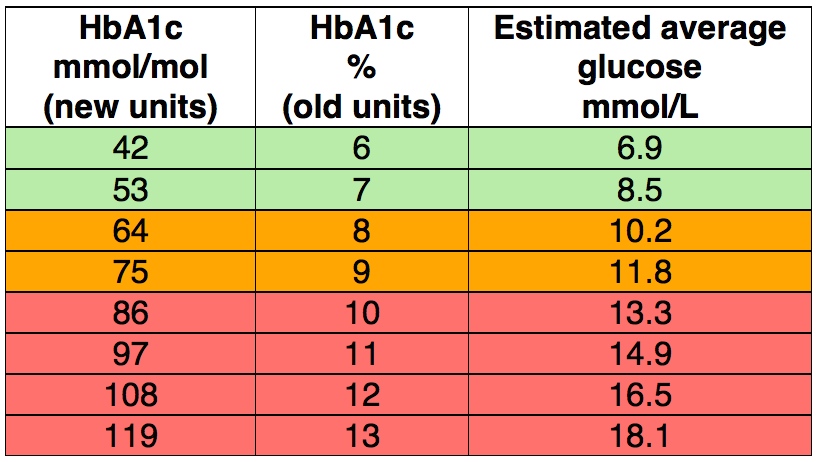
Over the last few years we have switched the units used to describe HbA1c from a percentage to mmol/mol. Although the test remains the same, the number reported is very different to what many patients have become used to over the years. The table below compares the old and new units, as well as describing what this means in terms of typical blood glucose readings (finger prick tests) – described as the ‘estimated average glucose’:
What is the diabetes clinic for?
The diabetes clinic serves two main purposes. The first, and most important, is in providing support to allow patients with diabetes to manage their condition. Most patients attend a diabetes clinic 2 or 3 times a year, however treatments such as insulin often require decision making several times each day. The main aim of the diabetes clinic is to provide patients with the information and education they require to effectively manage their diabetes.
The second aim of the clinic is to assess for complications of diabetes and ensure appropriate treatment is in place to prevent the development of complications or, when present, to prevent them from progressing. This is achieved by:
Ensuring blood glucose control is as good as it can be.
Ensuring blood pressure is within the normal range and, if not, starting appropriate treatment for blood pressure control.
Checking for protein in the urine - this can be an early sign of kidney damage and may be treated effectively with blood pressure lowering medication.
Annual foot examination to ensure there are no problems with sensation or blood supply.
Annual eye screening (by retinal photography) to detect any early signs of eye complications (known as retinopathy). Sometimes, where retinopathy has developed, patients benefit from specialist input from the eye hospital.
How often should I check my blood glucose level?
If you are not on insulin treatment then you may not actually need to check your blood glucose regularly. One significant exception to this is patients who drive and are on tablets which are capable of causing low blood glucose (hypoglycaemia). Your clinic doctor (or specialist nurse) will inform you if they feel glucose monitoring is appropriate. If you do not have a blood glucose meter and feel you should, please discuss this with a member of your diabetes team.
Patients on once or twice daily insulin would usually be advised to check their blood glucose level at least twice a day.
Patients on multiple daily injections of insulin (4 or 5 injections per day) are generally advised to check their blood glucose levels at least 4 times a day:
first thing in the morning before breakfast
before lunch
before evening meal
last thing at night before bed
It is well recognised that patients who check their blood glucose several times each day are more likely to achieve good control of their diabetes:
This table refers to a large group of people (approximately 3000) with type 1 diabetes in the United States, using multiple daily injections. It clearly demonstrates that more frequent blood glucose testing is associated with better diabetes control. For many patients with type 1 diabetes, checking blood glucose levels 4 times each day results in good overall control.
Diabetes 'control' – what difference does it make?
The goal of ECED diabetes clinics is to provide the support necessary to allow people to confidently manage their diabetes and lead as normal a life as possible. In addition we want to ensure that the risk of developing diabetes related complications is as low as possible.
Type 1 Diabetes
The best evidence for aiming to control blood glucose levels, comes from a large American study, The Diabetes Control and Complications Trial (DCCT), which started back in the early eighties. At that time it was not clear whether ‘tight’ control of blood glucose was important in reducing the risk of diabetes complications. Patients were randomly assigned to ‘conventional care’, which was typically twice-daily insulin injections, or ‘intensive insulin’ with multiple injections (4 per day). Over six years, patients in the intensive treatment group had an average HbA1c of approximately 7% (53 mmol/mol) compared to 9% (75) in the conventional group. This translated to a 76% reduction in the development of eye complications (retinopathy), a 39% reduction in kidney complications (microalbuminuria) and a 60% reduction in nerve problems (neuropathy). The results of this landmark study were published in the New England Journal of Medicine in 1993 and continue to inform our practice:
After this study finished, the conventional and intensive patients developed almost identical HbA1c levels (approximately 8% [64 mmol/mol]). Incredibly, even 30 years later, those who were allocated intensive treatment in the 1980s continue to have reduced rates of complications, a reduced risk of developing cardiovascular disease (e.g. heart attacks, strokes etc.) and a reduced risk of death. The results of the long-term follow up have been published in several leading medical journals:
Results of the long term DCCT follow up
Click here for a brief article describing the results of the DCCT
Type 2 Diabetes
Like the DCCT trial in type 1 diabetes, the United Kingdom Prospective Diabetes Study (UKPDS) was a huge project, which helped confirm that effective control of blood glucose levels is important in preventing the development of complications in patients with type 2 diabetes. Conventional treatment in this study was ‘dietary advice’ whilst intensive treatment included the use of medications or insulin. Intensive treatment resulted in an HbA1c of 7% (53 mmol/mol) compared to 7.9% (63 mmol/mol) in the conventional group. Over a ten year period, those patients in the intensive group had a significantly lower risk of developing diabetes complications:
Long term follow up of patients in the UKPDS has confirmed that intensive control is associated with a persistently lower risk of complications and also a reduced risk of heart attacks and death:
Link to long-term UKPDS follow up results
***INTENSIVE BLOOD GLUCOSE CONTROL IS NOT SAFE FOR ALL PATIENTS AND TARGETS SHOULD BE AGREED WITH A MEMBER OF THE DIABETES TEAM***
Reducing the risk of diabetes complications also involves ensuring blood pressure and blood cholesterol levels are appropriately managed. These important risk factors are considered during appointments at the diabetes clinic.
“I’m worried I’ll be told off at the clinic”
It is not uncommon to hear patients tell us that they were worried they’d be “told off” or “get a row” for having a high HbA1c. It is important to stress that HbA1c is a tool to help guide treatment and not a test that patients can pass or fail. It is quite normal to be apprehensive about your HbA1c result. No staff member at the ‘Edinburgh Centre for Diabetes and Endocrinology’ has been trained to sit in judgement of patients with higher than ideal HbA1c levels, our role is to offer constructive solutions to help people achieve a level of diabetes control that they are happy with.
What should I do when I'm unwell?
If you become ill (e.g. viral illness, vomiting, diarrhoea etc.) it is important to pay extra close attention to your blood sugar levels. This is particularly important for people on insulin and with type 1 diabetes. The following link, to My Diabetes My Way, provides useful information on what to do in this situation:
Sick day rules for Type 1 Diabetes
If you are ill and concerned about your sugar levels please contact your GP or the diabetes specialist nurses for advice.
How should I deal with hypos (low blood sugar)?
It is important to know how to correct a low blood sugar (less than 4 mmol/L) and the following link provides good advice:
If hypos are occurring regularly, it is important to work out why this is happening and aim to prevent it recurring. Please contact the nurse specialists if you would like further advice on avoiding hypoglycaemia.
Diabetes and alcohol
Advice on how alcohol affects glucose levels and how to keep safe when drinking
Driving and diabetes
Patients with car or motorcycle licenses do not need to inform the DVLA (Driver Vehicle and Licensing Agency) if they are not on insulin therapy. Patients with bus, coach or lorry licenses must inform the DVLA unless their only treatment is ‘diet’. Patients with diabetes should inform their motor insurance provider of their diagnosis. The following document explains the DVLA policy for people with INSULIN treated diabetes:
Should I be on a statin?
Statins are a class of medication, which lower blood cholesterol levels. They are highly effective in reducing the risk of cardiovascular disease (e.g. angina, heart attacks, strokes). Although reports in the press often raise the issue of side effects with statin therapy, the majority of patients tolerate this class of medication very well and the overall benefits, particularly in people with diabetes, far outweigh the potential risks. When side-effects occur, they are typically minor and generally respond to switching from one type of statin to another.
National guidelines suggest that most people with type 2 diabetes are likely to benefit from statin therapy. In type 1 diabetes, statins are suggested in patients over the age of 40 or where the overall risk of cardiovascular disease is elevated.
You can estimate your risk of developing cardiovascular disease using the ‘Q-intervention’ calculator – which also demonstrates the effect of a variety of interventions (including statins) on the risk of developing cardiovascular disease:
Q-intervention risk calculator
If you would like a full assessment of cardiovascular risk, please ask your clinic doctor to calculate your Q-Risk score.
Where else can I get help managing my diabetes?
Diabetes Nurse Specialists
The diabetes nurse specialists are available to offer telephone advice and to arrange face-to-face appointments between 9am and 5pm, Monday to Friday. If you have any diabetes-related questions or are concerned about your diabetes control, we would encourage you to get in touch.
Telephone: 01506 523 856/59 (SJH patients only)
This is an answer phone service. Please leave your name, date of birth and telephone number and someone will call you back. In the unlikely event that you do not receive a return telephone call within a 24 hour period, please call again.
DAFNE
DAFNE (Dose adjustment for normal eating) is a training programme for people with type 1 diabetes. All Edinburgh Centre for Diabetes & Endocrinology patients (Royal Infirmary of Edinburgh, Western General Hospital, St John’s Hospital, Leith Diabetes Clinic, Roodlands Diabetes clinic) with type 1 diabetes are potentially eligible for DAFNE, which involves a 5-day training course, designed to equip patients with the skills and confidence to effectively manage their diabetes. Patients who participate in DAFNE, irrespective of whether they have had diabetes for only a few years or for decades, generally find it a hugely positive experience. For more information please see the DAFNE website:
If you are interested in taking part in a DAFNE course, or would like to discuss it further, please contact your diabetes team or call the nurse specialists (contact details above)
My Diabetes My Way (MDMW)
‘My Diabetes My Way’ is an NHS Scotland interactive website to help support people with diabetes and their families. It contains a vast array of information (including leaflets and videos) covering many aspects of diabetes. Patients attending Scottish diabetes clinics also have the option of enrolling on to the MDMW website, where they can access their clinical information (blood pressure, HbA1c etc.) and diabetes clinic letters. For more information please visit the ‘My Diabetes My Way’ website:
Please ask your clinic doctor to arrange for you to be invited to join MDMW if you are interested (they can do this by taking your email address).
Dieticians
Referrals to the specialist diabetes dieticians are typically made by either clinic doctors or diabetes nurse specialists.